News & Articles

Demystifying Male Reproductive Cancers (Prostate, Testicular, Penile)

Often overshadowed by their female counterparts, male reproductive cancers carry their own weight of impact and importance.
ENSHROUDED IN MISCONCEPTIONS — such as the belief they only affect the elderly or that symptoms are always obvious — male reproductive cancers are a group of diseases that begin within the male reproductive organs. The American Centers for Disease Control and Prevention1 stress the importance of dispelling these myths, as understanding the realities of these cancers is critical for early detection and effective treatment. Knowledge is a powerful ally against the silent progression of these conditions, which are often hidden by a lack of symptoms until advanced stages.
PROSTATE CANCER
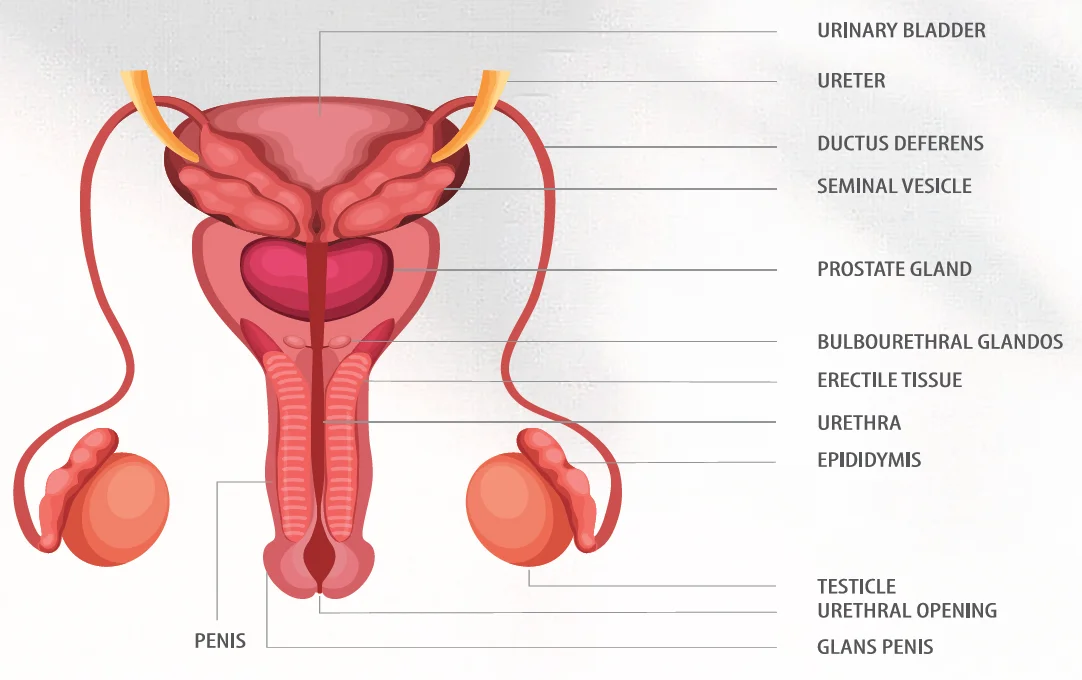
Prostate cancer is a cancer that occurs in the prostate. The prostate is a small walnut-shaped gland in males that produces the seminal fluid that nourishes and transports sperm.
How common is prostate cancer?
Prostate cancer is now the most common cancer among men in Singapore.
What are the risk factors?
The most common risk factors among Asians include:
- Age. Your risk increases as you get older. You’re more likely to get diagnosed if you’re over 50. About 60% of prostate cancers occur in people older than 65.
- Family history of prostate cancer. You’re two to three times more likely to get prostate cancer if a close family member has it.
- Genetics. You’re at greater risk if you have Lynch syndrome or if you inherited mutated (changed) genes associated with increased breast cancer risk (BRCA1 and BRCA2).
What are the signs and symptoms?
Prostate cancer is often asymptomatic in its early stages. Prostate cancer that is more advanced may cause signs and symptoms such as:
- Trouble urinating
- Decreased force in the stream of urine
- Blood in the urine
- Blood in the semen
- Bone pain
- Losing weight without trying
- Erectile dysfunction
Can I be screened for prostate cancer?
The goal of screening is to find cancers that may be at high risk of spreading if not treated, and to find them early before they spread.
A blood test called a prostate specific antigen (PSA) test measures the level of PSA in the blood. PSA is a substance made by the prostate. The levels of PSA in the blood can be higher in men who have prostate cancer. The PSA level may also be elevated in other conditions that affect the prostate. As a rule, the higher the PSA level in the blood, the more likely a prostate problem is present. But many factors, such as age and race, can affect PSA levels Some prostate glands make more PSA than others. Because many factors can affect PSA levels, your doctor is the best person to interpret your PSA test results. If the PSA test is abnormal, your doctor may recommend a biopsy to find out if you have prostate cancer.
It is recommended that you speak to your doctor about the pros and cons of prostate cancer screening.
How is prostate cancer treated?
Treatment options depend on various factors like the stage of cancer, overall health and personal preferences of the patient.
For localised prostate cancer, treatment options include:
- Active surveillance - Monitoring the cancer’s progression without immediate treatment.
- Surgery - Removing the prostate gland (prostatectomy) either through open or minimally invasive techniques like robotic-assisted surgery.
- Radiation therapy - Using high-energy rays to kill cancer cells, including external beam radiation and brachytherapy (internal radiation).
- Cryotherapy - Freezing cancer cells to destroy them.
- High-Intensity Focused Ultrasound (HIFU) - Using ultrasound waves to destroy cancer cells.
For advanced and metastatic prostate cancer, treatment options include:
- Hormone therapy - Lowering testosterone levels to slow cancer growth.
- Chemotherapy - Using drugs to kill cancer cells.
- Immunotherapy - Stimulating the immune system to fight cancer.
- Targeted therapy - Drugs targeting specific molecules involved in cancer growth.
The choice of treatment depends on the individual’s circumstances, and often a combination of therapies may be recommended. It is essential to discuss options thoroughly with your oncologists.
TESTICULAR CANCER
Testicular cancer is the growth of cancer cells that starts in the testicles. Also called testes, the testicles are found in the scrotum, which is a loose bag of skin underneath the penis. The testicles make sperm and the hormone testosterone.
How common is testicular cancer?
Testicular cancer is not a common cancer but it’s the most common cancer among young males aged between 15 and 35 years of age.
What are the risk factors?
Risk factors don’t cause testicular cancer, but they may increase its likelihood of developing the disease.
- Undescended testicles. Testicles form in the abdomen of a foetus during pregnancy and usually drop into the scrotum before birth. Testicles that don’t drop are called undescended testicles and may require surgery. Being born with this condition may increase your testicular cancer risk even if you have surgery.
- Personal or family history. You may be more likely to develop testicular cancer if a biological parent or sibling had it. Certain inherited genetic conditions, like Klinefelter Syndrome, may also increase the risk. Having testicular cancer in one testicle increases the likelihood of developing a second cancer in the other testicle.
What are the signs and symptoms?
The most common sign is a painless lump in your testicle. Other symptoms include:
- Swelling or sudden fluid build-up in your scrotum
- A lump or swelling in either testicle
- A feeling of heaviness in your scrotum
- Dull ache in your groin or lower abdomen
- Pain or discomfort in your scrotum or a testicle
How is testicular cancer treated?
Testicular cancer treatment often involves surgery and chemotherapy. Which treatment options are best for you depends on the type of testicular cancer you have and its stage.
Can testicular cancer be cured?
Testicular cancer is curable. While a cancer diagnosis is always serious, the good news is that it is treated successfully in 95% of cases. If treated early, the cure rate rises to 98%.
How does testicular cancer affect fertility?
Your doctor should talk to you about fertility before starting treatment. The effect on your fertility will depend on what treatment you need.
Most men have cancer in one testicle. You have surgery to remove the testicle. This doesn’t usually affect your ability to have children. But sometimes your remaining testicle might not work so well. This could reduce your fertility.
Chemotherapy for testicular cancer causes temporary infertility in most men. Usually fertility goes back to normal some months after the chemotherapy ends. But for some men, it doesn’t recover.
Your doctor will talk to you about sperm banking before you start your treatment.
PENILE CANCER
Penile cancer is when abnormal cells in the penis start to divide and grow in an uncontrolled way.
How common is penile cancer?
Penile cancer is rare in Singapore, accounting for less than 1% of cancers among men.
What are the risk factors?
Most men diagnosed with penile cancer are older than 50. The exact cause of penile cancer is not known but there are several risk factors including:
- Human papilloma virus (HPV). This is a common infection and it does not mean you will develop cancer of the penis. HPV type 16 and 18 are the most common type in penile cancers
- Having a weakened immune system. Penile cancer is more common in people with HIV.
- Smoking. The harmful substances in tobacco can damage cells in the penis.
- Phimosis. It’s a condition that causes your foreskin to become so tight you can’t pull it back to access the head of your penis.
What are the signs and symptoms?
Not all cancers cause changes you can see, but penile cancer usually causes your penis to look different. The skin on your penis may become discoloured, and you may notice a lump. Other signs and symptoms include:
- A growth or sore on your penis
- Bleeding or a foul smelling discharge
- A rash on your penis
- Difficulty pulling back your foreskin
- A change in colour of your penis or foreskin
- Lumps in the groin
Is penile cancer contagious?
Penile cancer isn’t contagious. However, HPV — one of the risk factors for penile cancer — is most often transmitted through skin-to-skin contact during unprotected sex. HPV spreads through vaginal sex, oral sex and anal sex.
How is penile cancer treated?
If found early, penile cancer can be treated with success and low risk. If the tumour is on top of the skin, it may be treated with a skin cream. This cream has few side effects. External beam radiation is also a therapy for small lesions.
If the lesion is larger — but still about the size of a pea — a small local excision or “Moh’s surgery” may be done. This is a type of surgery where layers of abnormal tissue are shaved off until normal tissue is reached. With both of these methods, the penis should still look normal and work as usual. But careful follow-up is vital to check for early recurrence. With small lesions, it is not likely that cancer has spread to the lymph nodes. For this reason, it is often not necessary to remove the lymph nodes.
With larger lesions, more tissue needs to be removed. Your surgeon will also consider taking out or draining lymph nodes in the groin. A mix of surgery, radiation and chemotherapy may be needed. In cases where the cancer is more advanced, the whole penis may need to be removed.
1Centers for Disease Control and Prevention, ‘Male Urologic Cancers,’ CDC, last modified 17 November 2020, https://www. cdc.gov/cancer/uscs/about/data-briefs/no21-male-urologic-cancers.htm.
| POSTED IN | Cancer Treatments |
| TAGS | common cancer, history of cancer, hormone therapy, men's cancer, metastatic cancer, misconceptions, prostatectomy, rare cancer, robotic surgery |
| READ MORE ABOUT | Prostate Cancer |
| PUBLISHED | 01 June 2024 |
