Pancreatic Cancer
Overview
What is Pancreatic Cancer?
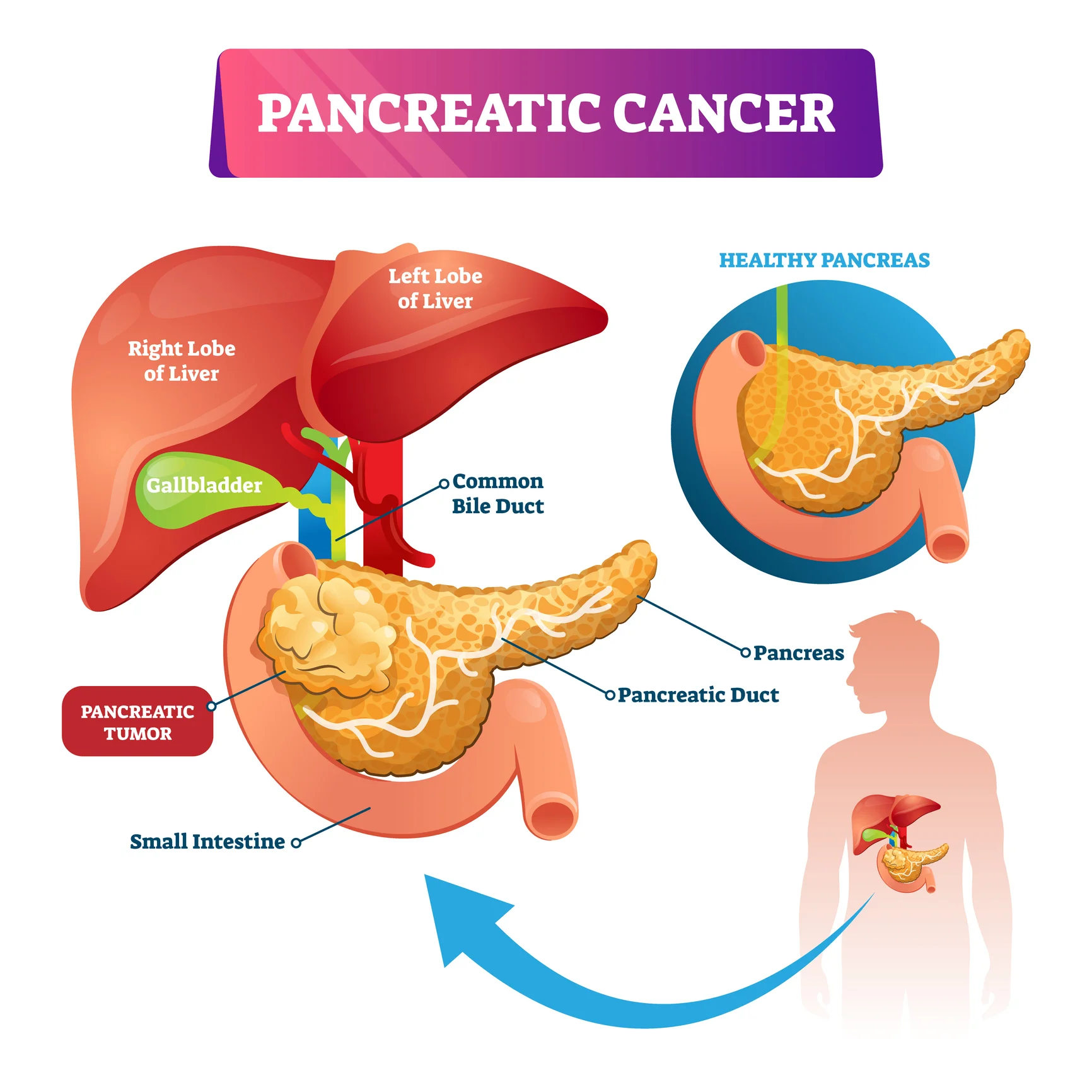
Pancreatic cancer is a disease in which malignant (cancerous) cells form in the tissues of the pancreas. The pancreas is an organ in the abdomen that lies horizontally behind the lower part of the stomach. Within the pancreas, exocrine pancreatic cells produce enzymes that help with digestion of food, while endocrine pancreatic cells produce the hormones insulin and glucagon, which regulate blood sugar levels in the body.
Pancreatic cancer is often difficult to detect and is diagnosed late for several reasons1:
- The early stages of pancreatic cancer tend to not show an signs or symptoms.
- The signs of pancreatic cancer, when present, are vague and similar to other more common abdominal conditions.
- The pancreas lies behind other organs in the abdomen which makes it difficult to visualise clearly on imaging tests.
Types of Pancreatic Cancers
Pancreatic cancers are categorised according to:
- The location of the cancer in the pancreas: The pancreas is made up of the head, body and tail. About 70% of pancreatic cancers are located in the head of the pancreas2.
- The type of cell that the cancer started from:
- One type of cell produces digestive enzymes that help in the digestion of food. These enzymes drain into ducts (tubes), which then drain into the small intestine. Cancer arising from the cells of these ducts is known as pancreatic exocrine cancer and is the most common form of pancreatic cancer, accounting for 95% of all pancreatic cancers.
- Another type of cell produces several important hormones such as insulin and glucagon that regulate blood sugar levels. Cancer in these cells is known as pancreatic neuroendocrine cancer and is much less common, accounting for about 1% of all pancreatic cancers3.
How Common is Pancreatic Cancer?
In Singapore, the incidence (number of cases) of pancreatic cancer has been steadily increasing over the past 50 years. It is the tenth most common cancer diagnosed in males and the 8th most common cancer in females. It is the fourth highest cause of cancer deaths in both males and females4.
The good news, however, is that the survival rate has improved over the same time period, in part due to a greater proportion of patients being diagnosed in the earlier stages of the disease4.
Causes & Symptoms
What causes Pancreatic Cancer?
Pancreatic cancer happens when cells in the pancreas develop changes (mutations) in their DNA that cause the pancreatic cells to grow abnormally and develop into a tumour. The exact trigger for the mutations are not fully known.
Pancreatic Cancer Risk Factors
There are certain risk factors that increase the chance of DNA damage in cells that may lead to pancreatic cancer. Such risk factors include2,5,6:
- Smoking: Smoking is the most important modifiable risk factor for pancreatic cancer. Heavy smokers are at greatest risk.
- Pancreatitis (inflammation of the pancreas): Having pancreatitis for a long time may increase the risk of pancreatic cancer.
- Type 2 Diabetes: People with diabetes are more likely than others to develop pancreatic cancer.
- Obesity: People who are overweight or obese, with a body mass index (BMI) >30 are slightly more likely than others to develop pancreatic cancer.
- Unhealthy diet: Consuming a diet high in fat or processed meat contributes to an increased risk for pancreatic cancer.
- Alcohol: A heavy intake of alcohol increases the risk of developing pancreatitis and pancreatic cancer.
- Chemical exposure: People in occupations that involve the heavy use of chemicals, such as pesticides, dye, metal-work and dry-cleaning chemicals, may be at increased risk.
- Family history: Having a first-degree relative (parent or sibling) with pancreatic, ovarian or colon cancer increases the risk of developing the disease. Some hereditary conditions that cause DNA changes can increase cancer risk. These include mutations in the BRCA2 gene, Lynch syndrome, familial atypical multiple mole melanoma (FAMMM) syndrome and multiple endocrine neoplasia type 1 (MEN1) syndrome.
- Older age: Most people with pancreatic cancer are over 65 years old.
- Gender: Men are more likely to develop pancreatic cancer.
Having one or more of these risk factors does not automatically mean that you will get pancreatic cancer. Many people with risk factors never develop pancreatic cancer, whilst some with no known risk factors do.
What are the Signs and Symptoms of Pancreatic Cancer?
Pancreatic cancer often does not cause symptoms until the disease is advanced. When they do occur, signs and symptoms of pancreatic cancer may include5,7:
- Abdominal (belly) pain that spreads to the sides or back
- Loss of appetite
- Unexpected weight loss
- Persistent fatigue or tiredness
- Indigestion
- Bloating
- Nausea and vomiting
- Jaundice (yellowing of the skin and the whites of the eyes)
- Light-coloured or floating stools
- Dark-coloured urine
- Itching
- New diagnosis of diabetes or diabetes that is difficult to control.
- Pain and swelling in an arm or leg, which might be caused by a blood clot
Diagnosis & Assessment
Diagnosis of Pancreatic Cancer
If pancreatic cancer is suspected, your doctor will investigate further to determine if you have cancer1,2,6:
- Clinical history and examination: Your doctor will ask about your personal and family medical history and perform a physical examination of your abdomen.
- Imaging tests: Imaging tests take detailed pictures that show the inside of the body. Tests used to diagnose pancreatic cancer include ultrasound, computed tomography (CT) scan, Magnetic resonance imaging (MRI) scans and positron emission tomography (PET) scans of the abdomen.
- Blood tests: Blood tests may show certain proteins called tumour markers that are produced by cancer cells. One tumour marker test used in pancreatic cancer diagnosis is called CA19-9. Doctors often repeat this test during and after treatment to understand how the cancer is responding. Some pancreatic cancers don't make extra CA19-9, so this test is not helpful for everyone. Other blood tests are also done to check your general health and how your kidneys and liver are functioning.
- Tissue biopsy: Biopsy is the removal of tissue samples to be viewed under a microscope to check for signs of cancer. The sample can be obtained through a fine needle or a core needle, which is inserted into the pancreas during an x-ray or ultrasound, or when the tumour is removed during laparoscopy or surgery. Specialised tests can show what DNA changes are present in the cancer cells.
- Endoscopic ultrasound (EUS): In this procedure, an ultrasound device is passed through a fibreoptic scope (endoscope) down the oesophagus and into the stomach in order to obtain images of the pancreas from inside the abdomen. A biopsy of the tumour can be taken during EUS.
- Endoscopic retrograde cholangio-pancreatography (ERCP): This procedure uses a fibreoptic scope (endoscope) to look into the stomach and small intestine where the ducts of the pancreas drain into. X-ray dye is injected into the ducts of the pancreas and images taken of the organ, allowing irregularities of the pancreatic ducts to be identified. During the ERCP procedure, tissues may also be biopsied.
- Percutaneous transhepatic cholangiography (PTC): A dye is inserted into the liver or bile ducts and then X-rayed to reveal any blockage. A PTC is usually performed if an ERCP is not possible.
How is Pancreatic Cancer Assessed?
After pancreatic cancer has been diagnosed, your doctor will determine the extent (stage) of the disease. Staging, usually done with CT scans, PET-CT scans or MRI, is done to find out whether the cancer has spread, and if so, to what parts of the body. Pancreatic cancer spreads most often to nearby blood vessels, lymph nodes, and then to the liver, peritoneum (the lining of your abdominal cavity) and lungs7. Unfortunately, the majority of pancreatic cancers have already spread beyond the pancreas at the time of diagnosis.
A staging laparoscopy may be done to determine the extent of pancreatic cancer and whether removal is possible. During this surgical procedure, a few small incisions (cuts) is made in your abdomen and a long tube with a camera on the end (scope) is inserted. This allows the surgeon to see inside your abdomen and look for abnormalities or signs of cancer spread. A biopsy or fluid sample from the abdomen may be taken during the procedure.
Genetic testing may be carried out on the biopsy material to identify any hereditary reason for your pancreatic cancer. It can help your doctor determine which type of treatment will be most effective for you.
Doctors describe pancreatic cancer stages as1:
- Stage 0: Abnormal cells are found in the lining of the pancreas. These abnormal cells may become cancer and spread into nearby normal tissue. Stage 0 is also called carcinoma in situ.
- Stage I: The tumour is smaller than 4cm and is found in the pancreas only.
- Stage II: The tumour is larger than 4cm or has spread to 1-3 lymph nodes nearby.
- Stage III: The cancer has spread to 4 or more lymph nodes or the major blood vessels around the pancreas.
- Stage IV: The cancer has spread to other parts of the body, such as the lung, liver, or peritoneal cavity (abdomen).
In order to facilitate treatment planning, another useful way to categorise pancreatic cancers is based on whether the tumour is resectable (removable by surgery) or not1,7:
- Resectable pancreatic cancer: The tumour can be removed by surgery because it has not grown into important blood vessels or organs nearby.
- Borderline resectable cancer: The tumour has grown into a major blood vessel or nearby tissue or organs. The tumour is removable but there is a chance that the cancer cells may not be removed completely.
- Locally advanced cancer: There is significant involvement of nearby blood vessels or lymph nodes. Surgical removal might be difficult or unsafe.
- Metastatic cancer: The cancer has spread to distant areas of the body, such as the liver, lungs or abdominal cavity. Surgery will not be able to completely remove the cancer.
- Recurrent cancer: The cancer has returned after it has been treated, either in the pancreas or other parts of the body.
Treatment of Pancreatic Cancer
Pancreatic Cancer Treatment Options
When considering your treatment plan your doctor will consider the following factors1,7:
- The exact location of the tumour.
- The stage of the cancer (the size of the tumour and whether it has spread beyond its original site).
- Whether the tumour can be removed by surgery.
- Your age, overall health and any other treatments you may have for other illnesses.
- Your preferences.
- Whether the cancer has just been diagnosed or has recurred (come back).
The first goal of pancreatic cancer treatment is to get rid of the cancer. When that is unachievable, the focus may be on stabilising the cancer to prevent its progression for as long as possible and improving quality of life. Pancreatic cancer can be treated with the following methods, often used in combination1,8:
Surgery: Early-stage pancreatic cancer can often be treated and possibly cured with surgery. For surgery to be successful, the cancer must be completely confined to the pancreas. Even then, there is still a chance that total cancer removal may not be possible7. After surgery, further treatment, known as adjuvant therapy, is often recommended. This may involve chemotherapy or radiotherapy.
However, many patients have advanced pancreatic cancer by the time it is diagnosed, and surgery in these cases is often not possible or beneficial9. If surgery is not recommended, treatment with radiotherapy, chemotherapy, or both are often used to shrink the cancer, reduce symptoms, and prolong life.
Surgical procedures used to treat pancreatic cancer include7,8:
- Surgery for cancers in the head of the pancreas: The Whipple procedure, also called pancreaticoduodenectomy, is an operation to remove the head of the pancreas, the first part of the small intestine, gall bladder and the bile duct. Part of the stomach and nearby lymph nodes may also be removed. The remaining organs are then rejoined to re-establish the digestive tract.
- Surgery for cancers in the body and tail of the pancreas: Surgery to remove the body and tail of the pancreas is called distal pancreatectomy. The spleen may also be removed.
- Surgery to remove the whole pancreas: This procedure is called total pancreatectomy and involves the removal of the entire pancreas, gallbladder, spleen and part of the stomach and small intestine. After surgery, you will need to take life-long medicines to replace the hormones and enzymes made by the pancreas.
If the cancer has spread and cannot be removed, palliative surgery may be performed to relieve symptoms and improve quality of life1:
- Biliary bypass: If cancer is blocking the bile duct and causing bile to build up in the gallbladder, a biliary bypass may be done. During this procedure, the surgeon will cut the gallbladder or bile duct in the area before the blockage and reattach it to the small intestine to bypass the blocked area.
- Endoscopic stent placement: A blocked bile duct can also be unblocked by placing a stent (a thin tube) through a tube that drains the bile into a bag on the outside of the body, or into the small intestine. This procedure is done under endoscopic (camera) guidance.
- Gastric bypass: If the tumour is blocking the emptying of food from the stomach into the duodenum (first part of the small intestine), the stomach may be sewn directly to the small intestine further along.
- Chemotherapy: Chemotherapy is the use of anti-cancer drugs to destroy cancer cells or stop them from dividing. Treatment may involve one chemotherapy medicine or a combination of them. Chemotherapy is often used after surgery to kill any cancer cells that might remain. Chemotherapy, with or without radiation therapy might be the first treatment used when surgery is not an initial option. Sometimes this combination of treatments shrinks the cancer enough to make surgery possible.
- Radiation therapy (or Radiotherapy): Radiotherapy uses powerful, high-energy beams to kill cancer cells. It can be used either before or after surgery and may be combined with chemotherapy. When the cancer spreads to other parts of the body, radiation therapy can help relieve symptoms such as pain by shrinking the tumour.
- Immunotherapy: Immunotherapy is treatment that uses the patient’s own immune system, or medications made from components of the immune system, to fight the cancer. Immunotherapy might be an option if your pancreatic cancer has specific DNA changes that would make the cancer responsive to these treatments.
- Targeted therapy: Targeted therapies are drugs that block the growth and spread of cancer by interfering with specific molecules involved in tumour growth and spread.
Pancreatic Cancer Survival Rate
The outlook for pancreatic cancer is unfortunately poor at present, as most cases are in the advanced stages by the time they are diagnosed. However, the overall survival rates for pancreatic cancer, while still much lower than other cancers, have gradually improved over the years4. The best outcome is seen in those who are diagnosed when the tumour is still confined to the pancreas and can be removed completely with surgery9.
It is worth noting that survival rates are grouped based on stage (how far the cancer has spread), but other factors such as your age, overall health and how well the cancer responds to treatment can also affect your prognosis (outcome). Even taking these things into account, the prognosis your doctor gives you will be an estimate based on the statistics we have of people who have had the same diagnosis. Your journey may still differ from another person’s in a similar situation.
Encouragingly, the proportion of early-stage diagnosis for pancreatic cancer has nearly doubled in recent years, indicating an improvement in earlier detection of the disease4. Furthermore, breakthroughs in cancer research are happening at a faster pace than ever before, providing greater insights and leading to the development of more effective treatment options. Researchers are working hard to find novel ways to improve the outcome and quality of life for those diagnosed with pancreatic cancer. You may wish to speak to your treating doctor to find out if there are clinical trials suited to your individual situation.
Prevention & Screening
Pancreatic Cancer Screening
Screening refers to looking for cancer before a person has any symptoms. Screening can help doctors find and treat pancreatic cancer early, when the cancer is localised and more easily removed by surgery. There is currently no recommended routine screening for the general population. However, people at high risk of getting pancreatic cancer, such as those with a strong family history of pancreatic cancer or hereditary DNA changes should be regularly monitored. Screening might involve imaging tests such as MRI and ultrasound of the abdomen repeated yearly, and genetic testing for relevant gene mutations depending on your family history5.
Pancreatic Cancer Prevention
While there is no guaranteed way to prevent pancreatic cancer, there are some measures you can take to reduce your risk6,7:
- Avoid or quit smoking: If you smoke, talk to a member of your health care team about ways to help you stop. These might include support groups, medicines and nicotine replacement therapy. It is estimated that after 10 years of quitting, your risk is the same as a person who has never smoked.
- Maintain a healthy body weight: A healthy diet and regular exercise can help you to keep to a healthy body weight and reduce your risk for many conditions including pancreatic cancer.
- Eat a healthy, balanced diet: A diet with less fat, sugar, red meat and processed foods, and more fresh fruits, vegetables and whole grains can help to reduce the risk of many diseases and cancers including pancreatic cancer.
- Limit or avoid alcohol consumption: Heavy alcohol use can cause pancreatitis, a risk factor for pancreatic cancer.
- Limit or avoid exposure to chemicals: Wear protective gear and observe occupational safety guidelines if you are exposed to cancer-causing chemicals in your workplace.
- Go for regular screening if you are in the high-risk group.
Frequently Asked Questions
Those with a family history of pancreatic cancer and inherited genetic mutations are at a significantly greater risk of getting pancreatic cancer. It is relatively rare, accounting for 5-10% of pancreatic cancer cases. Genetic testing and regular screening with imaging tests is recommended for people in this group.
Smoking is one of the biggest modifiable risk factors for pancreatic cancer. About 25% of pancreatic cancers are thought to be caused by cigarette smoking11.The chance of getting pancreatic cancer is about twice as high for people who smoke compared to those who have never smoked11. In addition, the combined effect of smoking, long-standing diabetes, and a poor diet increases a person’s risk of pancreatic cancer beyond the risk of any one of these factors individually6. If you currently smoke, the good news is that you can still reverse your risk if you quit smoking. It is estimated that after 10 years of quitting, your risk is the same as a person who has never smoked6.
Symptoms of pancreatic cancer are often vague and non-specific. Weight loss is a common first symptom, but it may not be attributed to pancreatic cancer at the outset as it is also a symptom of many other conditions. Many patients also report back or stomach pains as their first symptom. The pain would initially come and go and become worse after meals or when lying down7.
The 5-year survival rate in Singapore for someone with pancreatic cancer is 13%. This means that 13 out of 100 people with pancreatic cancer are alive five years after their diagnosis. This is largely due to the fact that most pancreatic cancers do not show symptoms until they have progressed to an advanced stage. If diagnosed and treated early (Stage 1), the 5-year survival rate can be over 60%.
It is important to understand that these statistical numbers are obtained from a group of people with the same diagnosis to represent an average. Individuals may differ in their own experience. It is best to discuss your prognosis (outcome) with your treating doctor who would be able to provide you with more specific information based on your personal circumstances.
Despite the overall poor outcome and the fact that it is mostly incurable, pancreatic cancer has the potential to be curable if caught and treated very early. Close to 10% of patients who are diagnosed in the early stages become disease-free after treatment12.
The best chance for a cure occurs when the tumour is truly contained in the pancreas (cancer cells have not spread elsewhere). However, this stage of disease accounts for less than 20% of cases as the cancer often only shows symptoms and signs when it has progressed to an advanced stage. For this small group of patients with localised disease and small tumours, complete surgical resection (removal) is associated with a 5-year survival rate of 18% to 24%9.The goal of ongoing research is to determine ways to detect a greater proportion of pancreatic cancer in its earliest stages when it is more likely to have a favourable treatment outcome.
References
- National Cancer Institute. Pancreatic Cancer Treatment (PDQ®)–Patient Version. Accessed at https://www.cancer.gov/types/pancreatic/patient/pancreatic-treatment-pdq on 31 May 2024.
- Cancer Council. Pancreatic Cancer. Accessed at https://www.cancer.org.au/cancer-information/types-of-cancer/pancreatic-cancer on 31 May 2024.
- Sing Health. Pancreatic Cancer. Accessed at https://www.singhealth.com.sg/patient-care/conditions-treatments/pancreatic-cancer on 31 May 2024.
- National Registry of Diseases Office. Singapore Cancer Registry Annual Report 2021. Singapore, National Registry of Diseases Office; 2022.
- Mayo Clinic. Pancreatic Cancer Symptoms and Causes. Accessed at https://www.mayoclinic.org/diseases-conditions/pancreatic-cancer/symptoms-causes/syc-20355421 on 31 May 2024.
- Mount Elizabeth. Pancreatic Cancer. Accessed at https://www.mountelizabeth.com.sg/conditions-diseases/pancreatic-cancer/symptoms-causes on 31 May 2024.
- Cleveland Clinic. Pancreatic Cancer. Accessed at https://my.clevelandclinic.org/health/diseases/15806-pancreatic-cancer#overview on 31 May 2024.
- Mayo Clinic. Pancreatic Cancer Diagnosis and Treatment. Accessed at https://www.mayoclinic.org/diseases-conditions/pancreatic-cancer/diagnosis-treatment/drc-20355427 on 31 May 2024.
- National Cancer Institute. Pancreatic Cancer Treatment (PDQ®)–Health Professional Version. Accessed at https://www.cancer.gov/types/pancreatic/hp/pancreatic-treatment-pdq on 31 May 2024.
- National Registry of Diseases Office. Singapore Cancer Registry 50th Anniversary Monograph – Appendices. Singapore, National Registry of Diseases Office; 2022.
- American Cancer Society. Pancreatic Cancer Risk Factors. Accessed at https://www.cancer.org/cancer/types/pancreatic-cancer/causes-risks-prevention/risk-factors.html on 31 May 2024.
- Johns Hopkins Medicine. Pancreatic Cancer Prognosis. Accessed at https://www.hopkinsmedicine.org/health/conditions-and-diseases/pancreatic-cancer/pancreatic-cancer-prognosis on 31 May 2024.
