Melanoma
Overview
What is Melanoma?
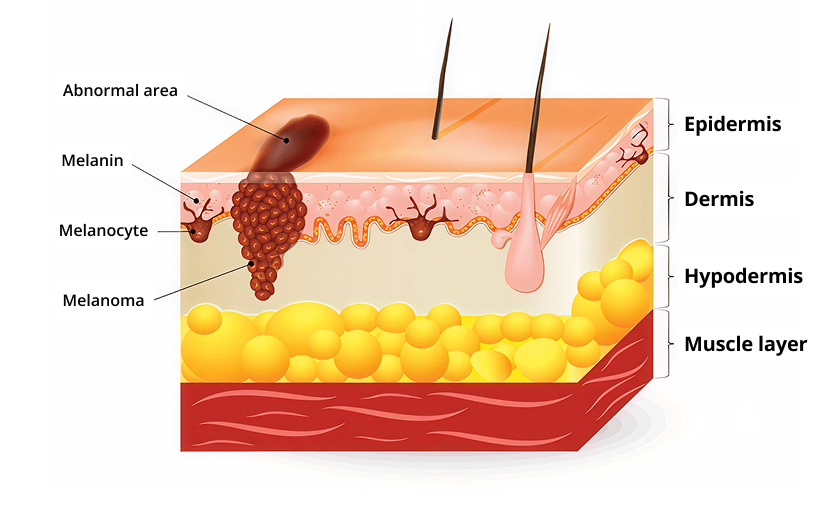
Melanoma is a disease in which malignant (cancerous) cells form in a particular type of skin cells known as melanocytes. Melanocytes are responsible for producing melanin, which is the pigment that gives skin its colour. These cells make more melanin when they are exposed to the sun in order to protect the deeper layers of the skin from the harmful effects of ultraviolet (UV) radiation1.
In Western countries, melanomas typically arise from sun-exposed areas of the skin such as the chest, forehead and limbs. However, in Asia they are more often seen in the hands and feet, which are less exposed to the sun, as well as in the internal mucosal lining of the mouth, nasal passages, rectum and vagina.2
Melanoma is much less common than other types of skin cancers such as squamous cell and basal cell cancers. But it is more dangerous because it is much more likely to spread to other parts of the body, especially if not found and treated early.3
Types of Melanomas
Most melanomas start in the skin and are called cutaneous melanomas. There are different types of cutaneous melanomas. The most common ones are3,4,5:
Superficial spreading melanoma: This is the most common type of melanoma seen in the Western population, accounting for the majority of cases. It tends to grow slowly across the skin first, before invading into the deeper layers of the skin. It can develop anywhere on the body but especially the trunk (central part of the body) in men, and legs in women.
Nodular melanoma: Nodular melanoma tends to grow downwards into the deeper layers of skin quickly and therefore are often found at a more advanced stage. It usually appears as a round, raised coloured lump (nodule) on sun-damaged skin. Up to 15% of melanomas are of this type.
Lentigo maligna melanoma: This type of melanoma may grow slowly and superficially for many years before growing deeper into the skin. It accounts for up to 15% of melanomas. It mostly appears as an abnormally shaped tan or brown spot in sun-damaged skin on the face, ears, neck or head.
Acral lentiginous melanoma: This is a rare form of melanoma in Western societies, but is the most common type seen in people with darker skin tones including those of Asian, African and Hispanic backgrounds. Unlike other melanomas, acral lentiginous melanoma is usually found in areas not exposed to the sun such as the palms of the hands, soles of the feet and under the nails. It generally has a poorer prognosis (outlook) than superficial spreading melanoma as it often goes undetected until it has reached an advanced stage.
Desmoplastic melanoma: Desmoplastic melanoma usually starts as a firm, growing lump, often the same colour as the skin and can look like a scar. It is mostly found on sun-damaged skin on the head or neck.
Melanomas can also rarely form in other parts of the body that have little or no exposure to the sun. These are referred to as hidden melanomas because they occur in places that most people would not think to check.
- Mucosal melanomas occur in the mucous membranes (internal lining) of the nose, mouth, throat, gastrointestinal tract and genitals.
- Ocular melanoma occurs in the eye, most commonly in the uvea (the middle layer of the eyeball). These are treated differently to cutaneous melanomas.
How Common is Melanoma?
Melanoma accounts for just under 2% of all cancers worldwide6. It is much more common is Western countries, particularly in Australia and New Zealand. It is rare in Singapore, where it makes up less than 0.5% of cancer cases diagnosed7.
Causes & Symptoms
What causes Melanoma?
Melanoma happens when melanocytes develop changes (mutations) in their DNA that cause them to grow abnormally and develop into a tumour. The exact trigger for the mutations is not fully known, but UV light is thought to be the cause for most melanomas that occur on sun-exposed skin. Other, as yet unclear factors lead to the development of melanomas in non-UV exposed areas.
Melanoma Risk Factors
Doctors may not always have an explanation as to why one person develops melanoma, and another does not. However, there are certain risk factors that increase the likelihood of a person developing melanoma, including8,9,10:
Exposure to ultraviolet (UV) light:
Up to 85% of melanomas worldwide are caused by UV rays11. UV radiation can come from the sun and also from tanning beds. People who live closer to the earth's equator or at higher elevations experience more intense sun rays and therefore are exposed to a higher amount of UV light. The UV Index is a measure of the intensity of solar UV rays through the course of a day. The scale ranges from Low (UV Index 0 to 2), Moderate (3 to 5), High (6 to 7), Very High (8-10) and Extreme (above 11). In Singapore, UV exposure is highest between 11am to 3pm and it is common for the UV Index to reach Very High and Extreme levels during this time period12.
Unprotected skin that is exposed to the sun when the UV Index is 3 or above can lead to permanent damage to the skin cells, especially with repeated exposure. You are more at risk if you have periods of short, intense sun exposure and sunburn, such as on weekends and holidays than if you have regular sun exposure from working outdoors.
Skin that sunburns easily: Melanoma can affect anyone, but you are more likely to get it if you have fair skin, blond or red hair, light-coloured eyes, freckles and a tendency to burn rather than tan.
Previous melanoma or other type of skin cancer: You are more likely to have another melanoma if you have had a previous melanoma or other skin cancer.
Having many moles or moles that are atypical: Having more than fifty moles on your body indicates an increased risk of melanoma, especially if they are large or have an irregular shape or colour.
Family history of melanoma: If a first-degree relative (parent, sibling or child) has or had melanoma, you have a greater chance of also developing it. This may be due to a shared family lifestyle of frequent sun exposure, an inherited tendency to have fairer skin, certain gene changes (mutations) that run in a family, or a combination of these factors9. Your risk is highest if your relative had melanoma when they were younger than 30 years old or if you have multiple first-degree relatives diagnosed with melanoma10.
Weakened immune system: People with a weakened immune system including those who need medicines to suppress the immune system, such as after an organ transplant, or have certain medical conditions, such as human immunodeficiency virus (HIV) infection, are at higher risk of developing melanoma.
What are the Signs and Symptoms of Melanoma?
Knowing the warning signs of melanoma can help ensure that the cancer is detected early and treated before it spreads. The first signs of melanoma are a change in an existing mole or the development of a new pigmented or unusual-looking growth on your skin.
To help differentiate a common, benign (non-cancerous) mole from a melanoma, check it against the following ABCDE characteristics8,11,13:
A is for Asymmetry: Are the halves of the mole different? Melanomas are more likely in moles with irregular shapes, where one half does not match the other.
B is for Border: Are the edges uneven, scalloped or notched? Look out for moles with irregular borders.
C is for Colour: Are there differing shades and colour patches? Melanomas often have uneven colour and may have different shades of black, grey, brown, pink or white. Normal moles usually have evenly distributed colour.
D is for Diameter: Is the mole greater than 5mm, or is it smaller than 5mm but growing larger? A mole larger than 5mm makes it more likely to be cancer.
E is for Evolution: Is the mole changing in appearance or size? Look for evolving changes such as a mole that has grown larger, changed in colour or shape, or is starting to ulcerate and bleed.
Another important sign, known as the ugly duckling sign, is a mole that stands out and looks different from all the other moles on your skin.
In Asian people, it is important to know the signs of acral lentiginous melanoma, which is the most common type of melanoma diagnosed in this population. Things to look out for include14:
- A darkened line or discolouration under your toenail or fingernail that may lead to nail damage.
- Any changing spot that may be growing on the hands or feet.
- A raised, thickened patch of skin on the sole of your foot or palm that may itch or bleed.
Melanomas vary greatly in appearance. Some may show all the changes listed above, while others may have only one or two warning signs. If you have one or more moles that you are concerned about, you should see your doctor promptly to have them checked out and treated if needed. Melanomas can be treated successfully with high cure rates if diagnosed early.
Diagnosis & Assessment
Diagnosis of Melanoma
If melanoma is suspected, your doctor will investigate further to determine if you have cancer5,8,15:
Clinical history and physical examination: Your doctor will ask about symptoms, risk factors and family history as well as have a careful look at your skin and feel for any enlarged lymph nodes (where the cancer may have spread to). A dermatoscope, which is a handheld magnifying instrument is used to examine a suspicious area more closely and see structures below the skin surface that is not visible to the naked eye. It can take digital images of the area which may be analysed by a computer to help the doctor determine if the mole is cancerous.
Tissue biopsy:
If your doctor suspects that a spot on your skin may be melanoma, the whole spot is removed (biopsied) to be analysed under a microscope. There are different methods to do a skin biopsy. Your doctor will choose the best option for you based on the size of the suspicious area, where it is on your body, the likelihood of scarring and other factors.
A skin biopsy is usually a simple procedure done in your doctor’s office using a local anaesthetic to numb the area. You may feel a little stinging as the anaesthetic is injected, but you should not feel any pain during the biopsy. The wound is then closed with small stitches and covered with a dressing. If you have an enlarged lymph node, your doctor may also biopsy the lymph node.
The tissue samples are analysed in a laboratory to determine whether melanoma cells are present. If melanoma is found, the pathologist (a specialist doctor who works in the laboratory) will look at certain important features such as tumour thickness and depth, number of cells that are actively dividing (known as mitotic rate) and whether the margins of the sample are clear of cancer cells. These features help your doctor determine how aggressive the cancer is and what further treatment is required.
Genetic testing may also be done on the cancer cells to look for specific protein or gene changes (mutations) such as the BRAF mutation gene which is found in about 40% of people with melanoma, and less commonly, the NRAS and C-KIT mutations5.
Blood tests: Blood tests to check your general health including your kidney, liver and bone marrow functions will be done. A test to measure the levels of an enzyme known as lactate dehydrogenase (LDH) may be done if the melanoma has spread to distant parts of the body. A high LDH level indicates that the cancer may be harder to treat.
How is Melanoma Assessed?
After melanoma has been diagnosed, you may undergo further testing to determine the extent (stage) of the disease. Melanoma spreads most often to lymph nodes, lungs, liver, bones and brain16. Staging tests may not be required for most people with very early-stage melanoma as the risk of it spreading is very unlikely. Tests that you may have include:
Imaging tests: Staging, usually done with bone scan, FDG PET-CT scan, CT or MRI scans are done to find out whether the cancer has spread, and if so, to what parts of the body.
Sentinel lymph node biopsy: If there are no clearly visible metastases (spread of cancer cells) noted on imaging studies or spread is suspected due to high-risk features, a sentinel lymph node biopsy may be done to check if there is microscopic spread to the lymph nodes. During a sentinel node biopsy, a radioactive dye is injected in the area where the melanoma was found. A special camera is used to track the flow of the dye into the nearby lymph nodes. The first lymph nodes to take up the dye (known as the sentinel lymph nodes) are removed and tested for cancer cells. If they are cancer-free, it is likely that the melanoma has not spread, and no further lymph node surgery is needed.
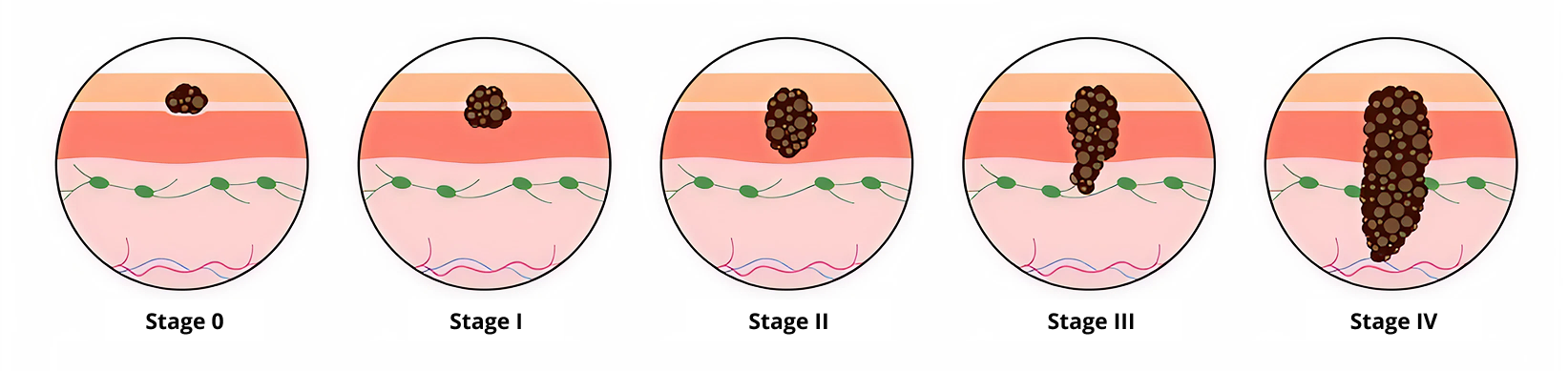
Early-stage melanomas have the highest chance of cure and best outcomes.
Treatment
Melanoma Treatment Options
When considering your treatment plan your doctor will take into account the following factors18:
- Location and size of the melanoma
- The stage (how far it has grown or spread)
- The depth or thickness of the melanoma
- Whether the cancer has specific gene changes (mutations)
- Your overall health and fitness level
- Your preferences
The first goal of melanoma treatment is to get rid of the cancer. Cure is likely if the cancer is detected early. The outlook for many patients with advanced melanomas has improved significantly with recent advances in treatment. However, in some cases of advanced melanomas, the focus may be on stabilising the cancer to prevent its progression for as long as possible and improving quality of life. Melanoma can be treated with the following methods, sometimes used in combination8,13,19:
Surgery: For melanomas that are small and thin, surgery might be the only treatment needed. If the melanoma has grown deeper into the skin, there is a risk that the cancer has spread. Therefore, other treatments are often used after surgery to kill any remaining cancer cells in the body. Surgical procedures used to treat melanoma include:
Wide local excision: This is surgery to remove the melanoma plus a margin of healthy tissue surrounding it to ensure that all the cancer is removed. Thin melanomas can often be cured with wide local excision alone.
Lymph node dissection (removal): If the melanoma has grown deeper into the skin or has spread to the nearby lymph nodes, surgery might be used to remove the lymph nodes.
Mohs surgery: This procedure might be an option for some very early-stage melanomas in areas where a wide excision might be difficult, such as the face or ears. During this procedure, the affected skin is removed in very thin layers which are then examined under a microscope. If cancer cells are present, the doctor removes another layer of skin. This process is repeated until a layer shows no signs of cancer.
Immunotherapy: Immunotherapy uses the body's natural defences to fight cancer by enhancing the immune system's ability to attack cancer cells. Examples of immunotherapies used to treat melanoma include:
PD-1, PD-L1 and CTLA-4 inhibitors: These drugs target certain proteins to boost the immune system and have brought about a breakthrough in the treatment of advanced melanomas. This has led to an improvement in the outcome for patients who previously had a poor outlook.
Oncolytic viruses: These are viruses that are altered in the laboratory to make them grow in cancer cells and destroy them, as well as boost the immune system to attack the cancer cells more effectively. The altered virus is injected directly into the melanoma and may be used in situations where the melanoma cannot be removed by surgery or has spread to lymph nodes or other skin areas.
Tumour infiltrating lymphocytes (TILs): More recently, TILs have been U.S. FDA approved for use in advanced melanoma. It is the first treatment for cancer that uses the patient’s own immune T-cells that have the ability to recognise and attack the cancer cells. TILs are collected from the patient’s tumour which is then expanded to large numbers in a laboratory before they are returned to the patient following a few rounds of “lympho-depleting” chemotherapy. Lymphodepletion is the process of reducing the other immune cells in your body to make room for the transferred TILs to work more effectively.
Targeted therapy: Targeted therapies are drugs that block the growth of cancer by interfering with specific molecules present in cancer cells that are involved in tumour expansion and spread. These therapies are used if the melanoma cells harbour specific cancer mutations such as BRAF mutations. It is used in cases where melanomas have spread to other organs or returned after treatment, as well as in the prevention of melanoma relapse following surgery in high-risk individuals (such as those with stage III resected melanoma).
Chemotherapy: Chemotherapy is the use of drugs to kill cancer cells or stop them from dividing. It is less often used to treat melanoma as more effective immunotherapy and target therapy drugs are now available. It might be an option to help control melanoma that doesn't respond to other treatments.
Radiation therapy (Radiotherapy): Radiotherapy uses powerful, high-energy beams to kill cancer cells. Radiotherapy may be used to treat melanoma that has spread to the lymph nodes, as further treatment for melanomas that could not be removed completely with surgery and to help relieve pain and other symptoms caused by melanoma that has spread to the brain or bone (palliative treatment).
Melanoma Survival Rate
The prognosis (outcome) for melanoma depends on multiple factors including19,20,21:
- Tumour characteristics (type of melanoma, thickness of the tumour, how quickly the cancer cells are dividing, whether there is ulceration).
- Location of the tumour on the body.
- Stage of the cancer (the extent of cancer spread) at diagnosis.
- The level of lactate dehydrogenase (LDH) in the blood.
- Whether the cancer has certain gene mutations (changes).
- How well the cancer responds to treatment.
- The patient's gender, age and general health.
Asians diagnosed with melanoma are more likely to have acral lentiginous type of melanoma, thicker tumours and more advanced disease state at time of diagnosis, ultimately resulting in an overall poorer prognosis14,21. Low awareness of the disease could also lead to delays in seeking diagnosis and treatment in this patient population.
Survival rates are better for women than it is for men across all stages of melanoma. The exact reason for this is unclear, but may be because women are more likely to see a doctor about their melanoma at an earlier stage20.
Compared to most other cancers, melanoma has a relatively good outlook for most patients, with an overall 5-year survival rate of 94%. The earlier it is diagnosed and treated, the better the outcome.
It is worth noting that survival rate statistics are measured every 5 years and therefore may not reflect the recent advances in melanoma treatment. People who are diagnosed with advanced melanoma now are likely to have a better prognosis (outcome) than these numbers show. Furthermore, breakthroughs in cancer research are happening at a faster pace than ever before, providing greater insights and leading to the development of more effective treatment options. Of note, early data from clinical trials of targeted therapy and combined immunotherapy have demonstrated 5-year survival rates of up to 50% for stage IV melanoma, which is a significant improvement for this group of patients23. You may wish to speak to your treating doctor to find out if there are clinical trials suited to your individual situation.
Survival rates are grouped based on stage (how far the cancer has spread), but other factors such as your age, overall health and how well the cancer responds to treatment can also affect your prognosis (outcome). Even taking these things into account, the prognosis your doctor gives you will be an estimate based on the statistics we have of people who have had the same diagnosis. Your journey may still differ from another person’s in a similar situation.
Prevention & Screening
Melanoma Screening
Screening refers to looking for cancer before a person has any symptoms. There is currently no recommended routine screening for melanoma for the general population. It is therefore important, especially if you have one or more risk factors (see Melanoma Risk Factors above) to be vigilant and see your doctor for prompt investigation if you notice any suspicious moles or spots.
Some people have a much higher risk of developing melanoma. This may include people who have24:
- Had more than 1 melanoma
- 2 or more first degree relatives (parent, sibling or child) who have had melanoma
- Had an organ transplant
- Dysplastic naevus syndrome
- An inherited gene abnormality or syndrome that increases the risk of melanoma
- A very large mole (bigger than 20cm across) from birth
If you have any of the above, it is recommended that you do monthly skin self-examinations as well as have regular appointments with a skin specialist (dermatologist) for total skin examinations and photographs (mole mapping) to closely monitor changes over time5.
Those with a strong family history of melanoma, personal history of several melanomas or melanomas at an early age, might be advised to go for genetic counselling and testing to see if they have a genetic mutation that increases their risk25.
Melanoma Prevention
Limiting exposure to UV radiation can help reduce the risk of melanoma and other skin cancers. Simple measures that you can take include5,12:
Avoiding the sun during the middle of the day: In Singapore, it is common for the UV Index to reach Very High and Extreme levels in the four-hour period between 11 am and 3 pm especially on days with little cloud cover. Avoid sunburn by minimising sun exposure and outdoor activities during this period when the UV radiation is most intense. If you must be out, seek shade where possible.
Wearing sunscreen year-round: Use a broad-spectrum sunscreen with an SPF of 30 or higher every day, even when it is cloudy. Apply sunscreen generously to ensure adequate coverage on all exposed skin and reapply every two hours, or more often if you are swimming or sweating. The recommended amount of sunscreen for an adult is 1 teaspoon for each arm, each leg, front of body, back of body, and 1 teaspoon for the face, neck and ears combined, which equates to 7 teaspoons of sunscreen for one full body application. Remember to protect your lips too by using a lip balm with sunscreen.
Wearing protective clothing: A UV Index of 3 or above indicates that UV levels are high enough to cause damage to unprotected skin, and you should use more than one type of sun protection. When you go outside during the day, wear a broad-brimmed hat that covers the head, neck and ears, sun protective clothing that covers your skin and close-fitting sunglasses that block UV light.
Avoiding solariums: Tanning beds and sun lamps give off artificial UV radiation and have been linked to increased risk of melanoma, especially if they are used before a person is 30 years old.
Being familiar with your skin so that you will notice changes: Check your skin regularly for new skin growths and look for changes in existing moles, freckles, spots and birthmarks. See your doctor promptly if you notice any worrying changes. (See What are the Signs and Symptoms of Melanoma? for further information)
Frequently Asked Questions (FAQ)
The first signs of melanoma are a change in an existing mole or the development of a new pigmented or unusual-looking growth on your skin. Being familiar with your skin will help you notice any changes more easily.
Some melanomas can grow quickly over months whilst others may take years to develop, depending on the type of melanoma and how advanced it is. Nodular melanomas tend to grow into the deeper layers of the skin quickly and therefore are often found at a more advanced stage. On the other hand, superficial spreading melanomas and lentigo maligna melanomas tends to grow slowly and superficially across the skin first, before eventually invading the deeper layers of the skin. (See Types of Melanomas for more detail on the different types of melanomas)
Melanoma has one of the best treatment outcomes among all cancers, especially if detected and treated early. An Australian study showed that patients who were diagnosed with thin melanomas (tumour thickness of 1mm or less) had a 20-year survival rate of 96%. This means that 96 out of 100 people with thin melanomas are alive twenty years after their diagnosis21.
Acral lentiginous melanoma, the most common type of melanoma in Asians has a poorer prognosis (outcome) as it tends to be diagnosed with thicker tumours and at more advanced stages. The 20-year survival rate for this type of melanoma is lower at 80%21, which is still a good outcome compared to many other cancers.
It is important to understand that these statistical numbers are obtained from a group of people with the same diagnosis to represent an average. Individuals may differ in their own experience. It is best to discuss your prognosis with your treating doctor who would be able to provide you with more specific information based on your personal circumstances.
Melanoma has an excellent outlook if treated early. Stage I and II melanomas are often cured with surgery alone.
References
- Cancer Research UK. What is Melanoma Skin Cancer? Accessed at https://www.cancerresearchuk.org/about-cancer/melanoma/about on 10 August 2024.
- Chang J, Guo J, Hung CY, et al. Sunrise in melanoma management: Time to focus on melanoma burden in Asia. Asia-Pacific Journal of Clinical Oncology. 2017; 13:423–427.
- American Cancer Society. What is Melanoma Skin Cancer? Accessed at https://www.cancer.org/cancer/types/melanoma-skin-cancer/about/what-is-melanoma.html on 10 August 2024.
- Cancer Research UK. Types of Melanoma. Accessed at https://www.cancerresearchuk.org/about-cancer/melanoma/stages-types/types on 10 August 2024.
- Cancer Council. Understanding Melanoma: A guide for people with cancer, their families and friends. Sydney, Cancer Council Australia; 2023.
- Sung H, Siegel RL, Laversanne M, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA: A Cancer Journal for Clinicians 2021; 71(3):209-49.
- The Global Cancer Observatory, International Agency for Research on Cancer, World Health Organization. Singapore Fact Sheet. Accessed at https://gco.iarc.fr/today/data/factsheets/populations/702-singapore-fact-sheets.pdf on 10 August 2024.
- Mayo Clinic. Melanoma. Accessed at https://www.mayoclinic.org/diseases-conditions/melanoma/symptoms-causes/syc-20374884 on 10 August 2024.
- American Cancer Society. Risk Factors for Melanoma Skin Cancer. Accessed at https://www.cancer.org/cancer/types/melanoma-skin-cancer/causes-risks-prevention/risk-factors.html on 10 August 2024.
- Cancer Research UK. Risks and Causes of Melanoma Skin Cancer. Accessed at https://www.cancerresearchuk.org/about-cancer/melanoma/risks-causes on 10 August 2024.
- Cleveland Clinic. Melanoma. Accessed at https://my.clevelandclinic.org/health/diseases/14391-melanoma on 10 August 2024.
- National Environment Agency. UV Radiation & UV Index. Accessed at https://www.nea.gov.sg/corporate-functions/weather/ultraviolet-index/uv-radiation-uv-index on 10 August 2024.
- Cancer Council. Melanoma. Accessed at https://www.cancer.org.au/cancer-information/types-of-cancer/melanoma on 10 August 2024.
- Melanoma Research Alliance. Acral Melanoma. Accessed at https://www.curemelanoma.org/about-melanoma/types/acral-melanoma on 10 August 2024.
- American Cancer Society. Tests for Melanoma Skin Cancer. Accessed at https://www.cancer.org/cancer/types/melanoma-skin-cancer/detection-diagnosis-staging/how-diagnosed.html on 10 August 2024.
- Cancer Research UK. About Advanced Melanoma. Accessed at https://www.cancerresearchuk.org/about-cancer/melanoma/advanced-melanoma/about-advanced-melanoma on 10 August 2024.
- Cancer Research UK. Melanoma Stages and Types. Accessed at https://www.cancerresearchuk.org/about-cancer/melanoma/stages-types on 10 August 2024.
- Cancer Research UK. Melanoma Treatment Options. Accessed at https://www.cancerresearchuk.org/about-cancer/melanoma/treatment/treatment-decisions on 10 August 2024.
- National Cancer Institute. Melanoma Treatment (PDQ®)–Patient Version. Accessed at https://www.cancer.gov/types/skin/patient/melanoma-treatment-pdq on 10 August 2024.
- Cancer Research UK. Survival for Melanoma Skin Cancer. Accessed at https://www.cancerresearchuk.org/about-cancer/melanoma/survival on 10 August 2024.
- Green A, Baade P, Coory M, et al. Population-Based 20-Year Survival Among People Diagnosed With Thin Melanomas in Queensland, Australia. Journal of Clinical Oncology 2012; 30(13):1462-1467.
- American Cancer Society. Survival Rates for Melanoma Skin Cancer. Accessed at https://www.cancer.org/cancer/types/melanoma-skin-cancer/detection-diagnosis-staging/survival-rates-for-melanoma-skin-cancer-by-stage.html on 10 August 2024.
- AIM at Melanoma Foundation. What are the Survival Rates for Melanoma? Accessed at https://www.aimatmelanoma.org/melanoma-101/how-melanoma-is-diagnosed/prognosis/ on 10 August 2024.
- Cancer Research UK. Screening for Melanoma Skin Cancer. Accessed at https://www.cancerresearchuk.org/about-cancer/melanoma/getting-diagnosed/screening on 10 August 2024.
- American Cancer Society. What Causes Melanoma Skin Cancer? Accessed at https://www.cancer.org/cancer/types/melanoma-skin-cancer/causes-risks-prevention/what-causes.html on 10 August 2024.