Blood Cancer
Overview
What is Blood Cancer?
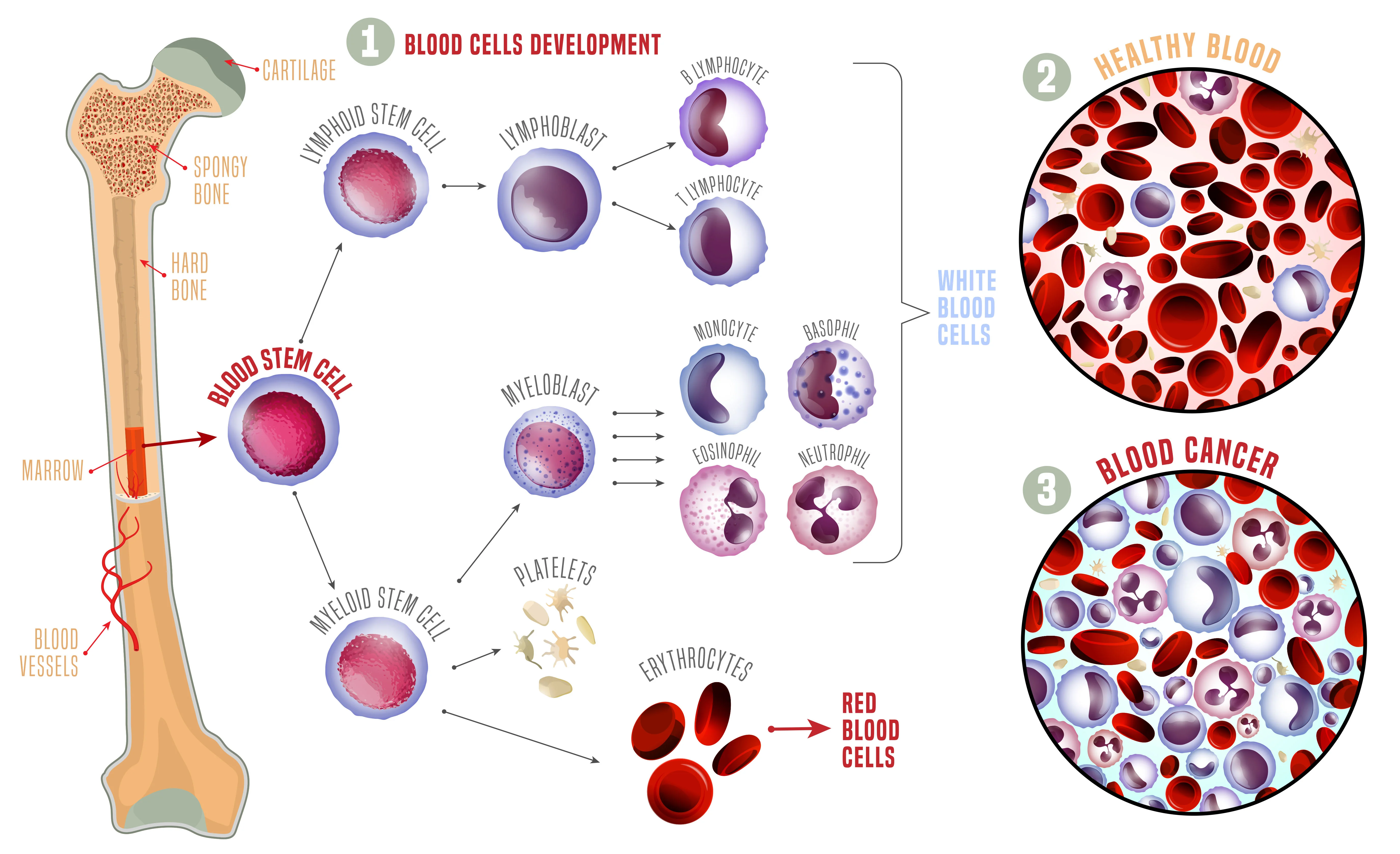
Blood cancer is a broad term that encompasses many different types of cancers that can affect your blood, bone marrow or lymphatic system.
Types of Blood Cancers
The most common types of blood cancers include:
Leukaemia is a type of cancer found in your blood and bone marrow, caused by the rapid production of abnormal white blood cells. These cells are not able to fight infections as normal white blood cells do and accumulate in the bone marrow interfering with the production of other normal blood cells1.
The main types of leukaemia can be grouped into four broad classifications based on the type of white cell affected (myeloid or lymphoid cell), and how the disease progresses (acute or chronic)2:
- Acute lymphocytic leukaemia (ALL)
- Acute myeloid leukaemia (AML)
- Chronic lymphocytic leukaemia (CLL)
- Chronic myeloid leukaemia (CML)
Acute leukaemia develops very quickly and requires immediate treatment, while chronic leukaemia progresses more slowly, and may not need treatment2.
Lymphoma is a type of blood cancer that affects the lymphatic system, which is responsible for removing excess fluids from your body and producing immune cells. It causes a type of white blood cells called lymphocytes to grow out of control, leading to swollen lymph nodes and growths throughout the body3.
The main types of lymphoma are Hodgkin Lymphoma and Non-Hodgkin Lymphoma. They can be further classified based on the type of lymphocytes affected (B-cell or T-cell). Some lymphomas are slow-growing and often do not cause symptoms or harm, whilst others can be aggressive, fast-growing lymphomas that cause symptoms quickly and require prompt treatment4.
Myeloma is a cancer of plasma cells, which are white blood cells that produce antibodies (also called immunoglobulins) to protect your body from infections. In myeloma, the abnormal plasma cells make only one type of antibody known as paraprotein, which has no useful function4. As the myeloma cells multiply and crowd out the bone marrow, the capacity to produce normal plasma cells and antibodies is reduced, thereby weakening the body’s immune system.
Different types and sub types of myeloma are based on the type of immunoglobulin (paraprotein) produced by the myeloma cell5.
How Common is Blood Cancer?
Lymphoid cancers (including lymphoma, myeloma, and lymphoid leukemia) as a group, is the fifth most common cancer seen in Singapore. It is the fourth most common cancer diagnosis in adult males and fifth in adult females6. Lymphoid cancer is the most common cancer diagnosed in both males and females under 30 years old, accounting for about 1 in 3 cancer diagnoses in the former, and 1 in 5 of all cases of cancer in the latter7.
Myeloid cancers (including acute and chronic myeloid leukaemia and myeloproliferative cancers) make up 2.7% of all cancers diagnosed in Singapore7. It is the ninth most common cancer diagnosed in adult males, but is less common in females6. Acute myeloid leukaemia accounts for about 30% of myeloid cancers7.
In children, blood cancers make up more than 50% of childhood cancers, with leukaemia accounting for 44% and lymphoma 10% of all cancers diagnosed in this age group8. Acute lymphoblastic leukaemia (ALL) is by far the most common childhood cancer, with 1 in 3 cancer cases attributable to it8.
Causes & Symptoms
What Causes Blood Cancer?
Blood cancer is thought to be caused by genetic changes (mutations) in the DNA within blood cells that cause them to multiply in an uncontrolled manner or live longer than they should9. Over time, these mutated cells can crowd out normal blood cells in the bone marrow, leading to reduced production of healthy white blood cells, red blood cells and platelets. These cancer cells also release substances called cytokines that attract other healthy cells to protect them and help them grow further. Crowding of the cells in the lymphatic system causes lymph nodes and organs such as the spleen to swell (enlarge).
Blood Cancer Risk Factors
Doctors may not always have an explanation as to why one person develops blood cancer, and another does not. However, there are certain risk factors that increase the likelihood of a person developing blood cancer, including3,9,10:
Age: Most blood cancers tend to occur in those aged over 65 years. An exception is acute lymphocytic leukaemia which is more common in children.
Sex: Males have a higher likelihood of developing blood cancers than females.
Ethnicity: In Singapore, people of Malay ethnicity have a higher incidence of blood cancers compared to their Chinese or Indian counterparts7.
Family history: Having a first-degree relative (parent or sibling) who has a history of leukaemia may increase your chance of developing it.
High levels of radiation: Exposure to high levels of radiation in the environment could lead to DNA damage and the development of blood cancers.
Chemical exposure: Cancer-causing chemicals such as benzene and formaldehyde can be found in building materials and household chemicals. Benzene is used to make plastics, rubbers, dyes, pesticides, drugs and detergents. Formaldehyde may be present in some building materials and household products such as soaps, shampoos and cleaning products.
Previous cancer treatment: Past cancer treatments involving radiation or chemotherapy may increase the likelihood of developing some types of blood cancers later on.
Immunosuppression: People who have a weakened immune system due to HIV infection, autoimmune diseases or medicines to suppress their immune system after an organ transplant, are at higher risk of some blood cancers.
Infections: Epstein Barr virus (EBV), human immunodeficiency virus (HIV) and Helicobacter pylori infections may increase the risk of lymphomas.
Genetic disorders: Certain genetic conditions such as Down Syndrome and Klinefelter Syndrome may increase your risk.
Smoking: A history of smoking or exposure to second-hand smoke puts you at increased risk of having a blood cancer.
How these factors affect risk depends on the type of blood cancer.
What are the Signs and Symptoms of Blood Cancer?
Blood cancer symptoms are often vague and non-specific. You may overlook early symptoms because they resemble symptoms of the flu and other common illnesses. Many people with early disease have no symptoms at all and it may be picked up as an incidental finding on routine blood tests.
People with blood cancer may experience a range of symptoms, including3,9:
Having any of these symptoms does not mean that someone has blood cancer. In fact, often these symptoms are not due to cancer. However, anyone with such symptoms should see a doctor to be diagnosed appropriately and treated if needed.
Diagnosis & Assessment
Diagnosis of Blood Cancer
The following tests and procedures may be performed to diagnose blood cancers11,12:
Physical examination: Your doctor will ask about your personal and family medical history and perform a physical examination for masses, such as swollen lymph nodes in your neck, underarm or groin, and enlarged spleen or liver.
Blood tests: A full blood examination and peripheral blood film will evaluate the number and appearance of your blood cells. Depending on the type of blood cancer suspected, you may have tests to measure the levels of difference enzymes and proteins in your blood. Your kidney and liver functions will also be checked to assess your general health.
Urine test: A urine collection may be analysed for the presence of protein.
Lymph node biopsy: This may be done in the form of an incisional biopsy (removal of a small piece of lymph node tissue) or excisional biopsy (removal of an entire lymph node). The tissue obtained is subjected to special stains that allow accurate classification of the cancer type.
Bone marrow aspiration and biopsy: This involves inserting a needle into your hip bone to remove a sample of fluid from the bone marrow and a biopsy needle to remove a small piece of the bone. The samples are analysed to look for cancer cells and the percentage of abnormal and normal cells.
How is Blood Cancer Assessed?
Once the diagnosis of blood cancer is confirmed, a staging assessment is carried out to determine the stage (extent) of the disease. Staging, usually with CT, MRI or PET scans, is done to find out whether the cancer has spread, and if so, to what parts of the body. A lumbar puncture (spinal tap) may also be carried out to obtain spinal fluid in order to determine if the cancer has spread to the central nervous system.
Genetic testing is usually done on cells collected from a blood test or a bone marrow biopsy to look for particular changes in the genes and chromosomes of the cancer cells in order to identify the specific type of blood cancer. Knowing if there are particular genetic changes (mutations) in your cancer cells can help to predict the best treatment choice for you, and give a clearer idea of your prognosis11.
Lymphoma is usually staged from Stage I (cancer is limited to one lymph node) to Stage IV (cancer has spread to multiple lymph nodes and other parts of the body), as well as an A or B category (depending on the absence or presence of recurrent fevers, night sweats or weight loss)13.
Leukaemia staging is a little bit different to conventional staging because leukaemia occurs in the developing blood cells in the bone marrow and is often already widespread throughout the body before the cancer is detected. The stages of leukaemia are often characterized by blood cell counts, cell subtype, genetic changes and the accumulation of cancer cells in other organs, like the liver or spleen, with each subtype staged using a system designed specifically for it14.
In myeloma, the stages range from 1 to 3, depending on certain protein and enzyme levels in your blood and presence of specific genetic changes. The stage tells your treating team how quickly your myeloma is growing. A stage 1 multiple myeloma grows at a slow rate, whereas a stage 3 multiple myeloma is aggressive and progresses quickly15.
Treatment of Blood Cancer
Blood Cancer Treatment Options
The goal of treatment is to destroy as many cancer cells as possible and bring the disease into remission, or if that is not achievable, to stabilise the disease to stop its progression for as long as possible. Complete remission is achieved when there are no signs of any cancer left in the body.
When considering your treatment plan your doctor will consider the following factors16:
- The subtype and stage of blood cancer you have
- Any genetic mutations you may have
- Your age, overall health and any other treatments you may have for other illnesses
- Any previous treatment(s) you have had for the cancer, and how you responded to that treatment
- Your personal preferences
There is a range of different treatments for blood cancer depending on the type of cancer you have. You might have one type of treatment or a combination of treatments. Common blood cancer treatments include17,18:
Chemotherapy: Chemotherapy drugs, also known as cytotoxics, represent the main treatment for most blood cancers. In general, these drugs kill cells that rapidly divide or grow. Whilst highly effective for killing cancer cells, they will also damage normal cells of the body which divide rapidly, like the hair follicles and normal blood-forming cells in the bone marrow, leading to side effects such as hair loss and temporary drop in blood cells (red blood cells, white blood cells, platelets). Other common side effects include fatigue, rash, nausea, vomiting, constipation or diarrhoea and mouth sores.
Targeted therapy: Targeted therapy is a tailored form of treatment that targets specific changes or substances in cancer cells that are driving the cancer cells’ growth. Targeted drugs can stop or switch off signals that make cancer cells grow, or can instruct the cancer cells to destroy themselves. Because of their targeted action on the cancer cells, these drugs mostly leave normal, healthy cells unaffected. Common side effects include diarrhoea, elevated liver enzymes, rash, high blood pressure, joint aches, fatigue and itchy eyes. Examples of targeted therapy used in blood cancers include monoclonal antibodies and small molecule drugs.
Immunotherapy: Immunotherapy is treatment that uses the patient’s own immune system, or medications made from components of the immune system, to fight the cancer. Whilst chemotherapy drugs exert their effect directly on the cancer cells, immunotherapy drugs work indirectly on the patients’ immune system. Hence, cancers may respond to chemotherapy very quickly, but it may take longer to see the effects if you receive immunotherapy alone. Common side effects include skin rashes, fatigue, diarrhoea, nausea, vomiting, flu-like symptoms and a drop in thyroid levels. Some types of immunotherapies may cause severe or fatal allergic and inflammation-related reactions, but these reactions are rare. Recent advances in research have led to the development of a significant number of new immunotherapy options, such as monoclonal antibodies that trigger the immune system, immune checkpoint inhibitors and CAR-T cell therapy.
Radiation therapy (Radiotherapy): Radiation therapy uses high-energy rays to kill cancer cells. It can shrink tumours and help to control pain. Radiation is sometimes used as first-line therapy in patients who have very large lymph node masses at presentation.
Bone marrow or stem cell transplants: A transplant of blood-forming stem cell allows a person to receive high doses of chemotherapy, radiation therapy, or both. The high doses destroy both cancer cells and healthy blood cells in the bone marrow. Following this, the patient receives a transfusion of healthy blood-forming stem cells that then develop into new blood cells. The stem cells may come from the patient (known as autologous stem cell transplantation) or from a healthy, matched donor (known as allogenic stem cell transplantation).
Supportive care: This includes treatments aimed at managing symptoms and side effects such as pain or nausea, low blood counts and infections.
If you have a slow-growing blood cancer, treatment may not be required straight away, and some people may never need it. This is called being on active surveillance, or “watch and wait”. You will undergo periodic tests and checks to monitor your condition and treatment may be initiated when the cancer starts to cause symptoms that interfere with your daily life, or if it turns into an aggressive form17.
Blood Cancer Survival Rate
It is best to discuss your prognosis (outlook) with your treating specialist as they would be able to give you advice that is specific to your situation based on the information that they have about your cancer.
Your individual prognosis will depend on several factors, including9:
- Your diagnosis, including the type of blood cancer and the results of genetic tests
- The stage of the cancer at diagnosis
- Your age and general fitness
Even taking these things into account, the prognosis your doctor gives you will be an estimate based on the statistics we have of people similar to you who have had the same diagnosis. Your journey may still differ from another person’s in a similar situation.
Prevention & Screening
Blood Cancer Screening
Screening refers to looking for cancer before a person has any symptoms. The aim is to detect cancers early so that it can be treated at an early stage when treatment is likely to be more effective. There is no recommended screening tests for blood cancers as there is no effective and accurate test that is available currently.
In the absence of a routine screening test, it is important for people who have risk factors for blood cancer to be especially vigilant for possible symptoms and to consult promptly with a doctor regarding anything that seems out of the ordinary.
Blood Cancer Prevention
Few of the known risk factors for blood cancers can be changed, so it is not possible to prevent most cases of the disease at this time.
However, stopping smoking, avoiding exposure to cancer-causing chemicals, such as benzene and formaldehyde, and unnecessary exposure to radiation is generally good practice.
Frequently Asked Questions (FAQ)
Blood cancer and its treatment can impact your general health and wellbeing. You may be constantly tired, susceptible to frequent infections and feel down or worried about your diagnosis. You could suffer some side effects from treatment such as nausea, loss of appetite and mouth ulcers. Here are some suggestions that may help improve your sense of wellbeing18:
Aim to have a sensible, well-balanced diet with plenty of fruit and vegetables, healthy sources of protein, wholegrains, healthy fats, dairy and enough fluids. Your doctor can refer you to a dietician to help you with strategies to improve your intake of nutritionally dense foods.
Protect yourself from infection. Practise good hand hygiene and wear a mask if you have to be in a crowded area.
Aim to exercise regularly but ensure that you are not pushing yourself too hard. Gentle exercise such as walking is recommended.
Pay attention to your body and rest when you need to. Pace your activities so that they are spaced out with periods of rest in between.
Look after your emotional health. It is understandable if you feel overwhelmed, depressed or anxious about your situation. Explore new ways to improve your mental wellbeing, such as mindfulness activities, journaling, yoga and social activities with loved ones. Talk to your doctor if your mood is persistently low, you are unable to enjoy things that you used to, or if it affects your ability to function in your daily life.
Some people live for years with blood cancer. It is not always easy to navigate a chronic (long-term) condition. A support group where people with similar diagnosis to yours meet together can be a great source of comfort, support and practical suggestions.
Immunotherapy and targeted therapy remain in the forefront of blood cancer treatment advancement in recent years. New drugs are being developed and approved faster than ever before, leading to an exciting increase in treatment options, particularly for those cancers that have previously been difficult to treat or have a poor outcome.
Bispecific antibodies and CAR-T cell therapy are examples of the recent breakthroughs in immunotherapy that are already making a significant positive change in the outcome of some blood cancers. Researchers are also looking into refining and expanding the use of these treatments to benefit more patients. Discovery of new target proteins on blood cancer cells are occurring constantly and this will expand the number of potential sites for new cancer drugs to act on.
In addition to the innovative therapeutic advances, novel tests that provide greater precision in diagnosis and prognosis are emerging to better guide individualised treatment. For example, new blood tests, known as “peripheral biomarkers”, are being developed that can predict the best time to stop and if necessary, to restart treatments. These tests would reduce the likelihood of unnecessary treatment and the need for more invasive tests.
Certain blood cancers have some of the best cancer survival rates. For example, the overall 5-year survival for Hodgkin lymphoma is around 89%, and unlike other cancers, many late stage or advanced cases still have a good survival rate of over 80%19. Significant advances in the treatment of childhood leukaemia in Singapore has also led to an improvement in outcome, with more than 80% of affected children being long-term survivors and considered cured20.
It is worth noting that survival rates are grouped based on stage (how far the cancer has spread), but other factors such as your age and overall health and how well the cancer responds to treatment can also affect your prognosis (outlook)21. They cannot predict what will happen in a particular individual’s case.
Blood cancers have some of the best cure rates amongst cancers. The goal of blood cancer treatment is often to cure the condition. However, when cure is unlikely, there is a growing number of treatments that may place some blood cancers into remission. Remission means there is no cancer signs and symptoms for a long time.
Almost 9 in 10 people with classical Hodgkin lymphoma respond well and go into remission after first-line treatment13. Unlike other types of cancer, you can still go into remission in advanced stage (3 or 4) disease.
References
- Leukaemia Foundation. Leukaemia. Accessed at https://www.leukaemia.org.au/blood-cancer/types-of-blood-cancer/leukaemia/ on 24 May 2024.
- American Society of Hematology. Leukemia. Accessed at https://www.hematology.org/education/patients/blood-cancers/leukemia on 24 May 2024.
- Mayo Clinic. Lymphoma Symptoms and Causes. Accessed at: https://www.mayoclinic.org/diseases-conditions/lymphoma/symptoms-causes/syc-20352638 on 24 May 2024.
- Lymphoma Australia. What is Lymphoma? Accessed at https://www.lymphoma.org.au/lymphoma/what-is-lymphoma/ on 24 May 2024
- Myeloma Australia. What is Myeloma. Accessed at https://myeloma.org.au/what-is-myeloma/ on 24 May 2024.
- National Registry of Diseases Office. Singapore Cancer Registry Annual Report 2021. Singapore, National Registry of Diseases Office; 2022.
- National Registry of Diseases Office. Singapore Cancer Registry 50th Anniversary Monograph (1968 – 2017). Singapore, National Registry of Diseases Office; 2018.
- National Registry of Diseases Office. Singapore Childhood Cancer Registry (2003-2007). Singapore, National Registry of Diseases Office; 2008.
- Blood Cancer UK. About Blood Cancer. Accessed at https://bloodcancer.org.uk/understanding-blood-cancer/ on 24 May 2024.
- Cleveland Clinic. Leukemia. Accessed at https://my.clevelandclinic.org/health/diseases/4365-leukemia on 24 May 2024.
- Blood Cancer UK. Blood Cancer Tests. Accessed at https://bloodcancer.org.uk/understanding-blood-cancer/tests-diagnosis/ on 24 May 2024.
- Mayo Clinic. Lymphoma Diagnosis and Treatment. Accessed at https://www.mayoclinic.org/diseases-conditions/lymphoma/diagnosis-treatment/drc-20352642 on 24 May 2024.
- Lymphoma Australia. Hodgkin Lymphoma. Accessed at https://www.lymphoma.org.au/types-of-lymphoma/hodgkin-lymphoma/ on 24 May 2024.
- Cancer Center. Leukemia Stages. Accessed at https://www.cancercenter.com/cancer-types/leukemia/stages on 24 May 2024.
- Mayo Clinic. Multiple Myeloma Diagnosis and Treatment. Accessed at https://www.mayoclinic.org/diseases-conditions/multiple-myeloma/diagnosis-treatment/drc-20353383 on 24 May 2024.
- Lymphoma Australia. What is Lymphoma. Accessed at https://www.lymphoma.org.au/lymphoma/what-is-lymphoma/ on 24 May 2024.
- Blood Cancer UK. Blood Cancer Treatment Types. Accessed at https://bloodcancer.org.uk/understanding-blood-cancer/treatment/blood-cancer-types-treatment/ on 24 May 2024.
- Cleveland Clinic. Blood Cancer. Accessed at https://my.clevelandclinic.org/health/diseases/22883-blood-cancer on 24 May 2024 on 24 May 2024.
- Surveillance, Epidemiology and End Results Program, National Cancer Institute. Cancer Stat Facts: Hodgkin Lymphoma. Accessed at https://seer.cancer.gov/statfacts/html/hodg.html on 24 May 2024.
- National University Cancer Institute Singapore. Accessed at https://www.ncis.com.sg/Cancer-Information/About-Cancer/Pages/Paediatric-Cancer.aspx#:~:text=The%20Leukeamia%20cells%20also%20escape,Singapore%20and%20throughout%20the%20world on 24 May 2024.
- American Cancer Society. Survival Rates for Hodgkin Lymphoma. Accessed at https://www.cancer.org/cancer/types/hodgkin-lymphoma/detection-diagnosis-staging/survival-rates.html on 24 May 2024.